This purpose‐built, cloud‐based payer solution supports health plans, third-party administrators (TPAs) accountable care organizations (ACOs), independent physician associations, and other large at-risk managed care organizations. Designed to automate and integrate core administration, population health, and medical management under one easy‐to‐use rules-based, data-driven plaƞorm, the Advalent plaƞorm enables health care organizations to minimize the total cost of maintaining traditional Commercial, Medicare, Medicaid and Exchange lines of business while helping them transition to value‐based payment models. And, with implementaƟons that take days rather than months, Advalent not only gets you online and more efficiently sooner, but also has the added benefit of making life a little easier for your IT departments. Our core team, consisting of experts/leaders who have worked in Health Plans, assists health plans in business management consultancy and advisory capacity.
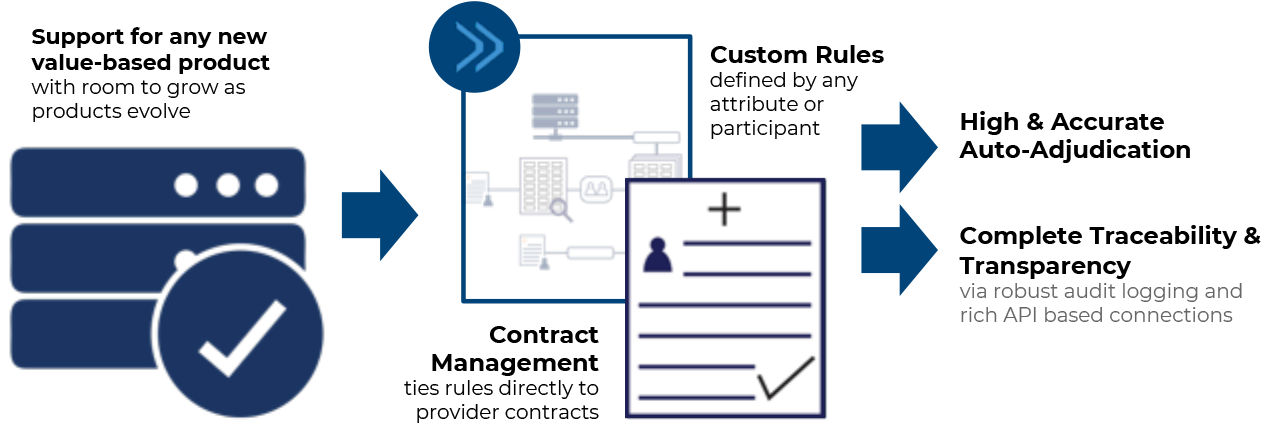
Despite millions invested in complex auto-adjudication systems, payers continue to have to manually interpret and troubleshoot common claim submissions, inaccurate payments, and member complaints. To pay claims accurately, they need accurate data and interconnected systems which allow for flexibility and growth. Advalent’s adaptable, rules-based core claims administration solution is designed to handle the most complex value-based products with simple, editable rules and real-time adjudication.